Clinic for Implant
&
Orthodontic Dentistry, procedures explained, offers, information,
PMMA vs. Zirconia in All-on-4 Bridges: Why We Prefer PMMA for Full-Jaw Restorations - By Dr Amir Mostofi DDS, Dip. (Ortho.) , MSc (Implant.)
When selecting materials for All-on-4 implant bridges, our practice favours Poly(methyl methacrylate) (PMMA) over zirconia for full jaw restorations. This preference stems from PMMA's ability to be crafted with multiple layers, resulting in a more natural and lifelike appearance. Additionally, PMMA's lightweight nature offers enhanced comfort compared to the denser zirconia, which some patients may find heavier. Furthermore, PMMA bridges are easily repairable and more cost-effective, whereas zirconia bridges, though durable, can be challenging and expensive to fix if damaged. Therefore, PMMA presents a practical and aesthetically pleasing choice for patients seeking full jaw implant solutions.
When considering All-on-4 implant bridges—a dental procedure where a full arch of teeth is supported by four implants—it's essential to choose the right material for the prosthetic teeth. Two commonly used materials are poly(methyl methacrylate) (PMMA, a type of acrylic) and zirconia (a type of porcelain). At our practice, we have chosen to use PMMA for full jaw construction implant bridges. Here's why:
1. Aesthetics and Natural Appearance
High-quality PMMA teeth are typically crafted with multiple layers, allowing for a more natural and lifelike appearance. This layering technique enables dental technicians to mimic the translucency and shading variations found in natural teeth. In contrast, zirconia prosthetics are usually milled from a single layer, which can result in a more uniform and less natural look. Therefore, PMMA offers superior aesthetics, providing patients with a smile that closely resembles natural dentition.
2. Weight and Comfort
PMMA is a lightweight material, contributing to a more comfortable experience for patients. Zirconia, being denser, results in a heavier prosthesis. Some patients may find the additional weight of a zirconia bridge less comfortable, especially during the initial adjustment period. The lighter nature of PMMA can enhance overall comfort and adaptability. All On Four
3. Occlusal Considerations
When zirconia is used for both upper and lower bridges, patients may experience a clicking sound due to the contact between two hard surfaces, similar to the sound of porcelain teeth clashing. This phenomenon can be distracting and may affect the overall satisfaction with the prosthesis. PMMA, being a softer material, does not produce such noises, leading to a more natural and quiet biting experience. Dr. Sehmi
4. Repairability and Maintenance
One significant advantage of PMMA is its reparability. If a PMMA bridge chips or fractures, it can be easily and cost-effectively repaired without the need for extensive procedures. In contrast, zirconia bridges, while durable, are challenging to repair if damaged. A fracture in a zirconia prosthesis often necessitates the fabrication of an entirely new bridge, leading to increased costs and inconvenience for the patient.
5. Cost-Effectiveness
PMMA bridges are generally more affordable than their zirconia counterparts, making them an attractive option for patients seeking quality restorations without incurring high expenses. The lower cost does not compromise the aesthetic and functional outcomes, especially when considering the advanced layering techniques used in modern PMMA prosthetics.
Conclusion
While both PMMA and zirconia have their respective advantages, our practice has chosen to utilize PMMA for full jaw construction implant bridges due to its superior aesthetics, comfort, reparability, and cost-effectiveness. These factors align with our commitment to providing patients with natural-looking, durable, and affordable dental restorations.
For more information and a consultation visit, call us on 0190-821822 or visit our practice at 7 Chapel Road, Worthing BN111EG.
Closing the Gap: Effective Orthodontic Solutions for Gaps Between Upper Front Teeth (Midline Diastema) in Worthing, West Sussex - By Dr Amir Mostofi DDS, Dip. (Ortho.), MSc (Implant).
Do you have a gap between your upper front teeth (midline diastema) and wonder if orthodontic treatment can help? Many people feel self-conscious about this common dental issue, but modern orthodontic solutions can effectively close the gap and enhance both function and aesthetics. Whether you prefer braces, clear aligners, or cosmetic treatments like bonding or veneers, our expert team in Worthing, West Sussex, offers tailored solutions to meet your needs. Discover the causes of these gaps, treatment options, and how to maintain a beautifully aligned smile. Book your free consultation today and take the first step towards a confident new smile!
Are you self-conscious about the gap between your upper front teeth (midline diastema)? This common dental concern can affect both appearance and confidence. Fortunately, modern orthodontic treatments offer effective solutions to close this gap and give you a beautifully aligned smile. If you’re in Worthing, West Sussex, and looking for expert orthodontic care, our clinic is here to help.
What Causes Gaps Between Upper Front Teeth?
A gap between the upper front teeth (midline diastema) can occur due to various reasons, including:
- Genetics – If your family members have gaps in their teeth, you may inherit the same trait.
- Oversized Labial Frenum – The tissue connecting your upper lip to your gums may extend between your front teeth, preventing them from coming together.
- Mismatched Jaw and Tooth Size – When teeth are too small compared to the jawbone, spaces may appear between them.
- Habits and Oral Health Issues – Thumb sucking, tongue thrusting, or gum disease can contribute to the development of a gap between the teeth.
Why Should You Close the Gap?
While some people embrace their gap as a unique characteristic, others may feel self-conscious about it. Additionally, gaps between teeth can sometimes lead to oral health issues, including:
- Misalignment of Surrounding Teeth – Extra space can cause other teeth to shift, leading to bite problems.
- Difficulty Biting and Chewing – Gaps may affect how the teeth come together when eating.
- Increased Risk of Food Getting Stuck and Plaque Build-up – Gaps create extra spaces where food particles can get trapped, leading to a higher risk of cavities and gum disease.
- Speech Difficulties – Some people may develop a slight lisp due to improper tongue positioning.
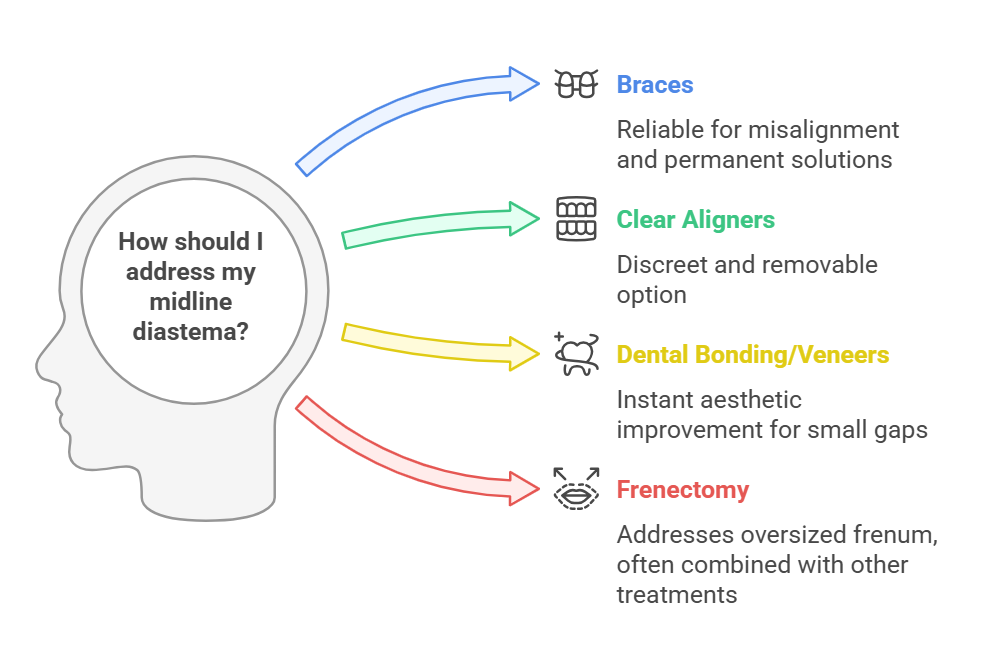
Orthodontic Treatments to Close the Gap
At our Worthing-based orthodontic clinic, we provide customised treatment options to help close gaps between the upper front teeth (midline diastema) effectively:
1. Braces
Traditional metal braces or ceramic braces use gentle pressure over time to bring the teeth together. Braces remain one of the most reliable and permanent solutions for closing gaps between teeth. This method is especially effective for patients who have additional misalignment or bite issues.
2. Clear Aligners
For those looking for a more discreet treatment, Invisalign® clear aligners are an excellent alternative. These removable, nearly invisible trays gradually shift the teeth into alignment without the need for metal brackets or wires. Many patients in Worthing prefer Invisalign® because it allows them to maintain their confidence while undergoing treatment.
3. Dental Bonding or Veneers
For smaller gaps, cosmetic solutions like dental bonding or porcelain veneers may be an option. These treatments provide an instant aesthetic improvement but do not correct underlying alignment issues. Bonding is a quick and affordable option, while veneers offer a longer-lasting solution for those who want a flawless smile.
4. Frenectomy (If Necessary)
If an oversized labial frenum is the cause of your gap, a minor surgical procedure known as a frenectomy can help. This is often combined with orthodontic treatment to ensure long-term results. Without addressing the root cause, gaps may reopen even after orthodontic intervention.
How Long Does Treatment Take?
The duration of treatment depends on the method chosen and the severity of the gap:
- Braces – Typically, 6 to 12 months.
- Invisalign® – Around 6 to 12 months, depending on the case.
- Dental Bonding – Completed in a single appointment.
- Veneers – Requires two or more appointments.
- Frenectomy – A short procedure followed by healing time, after which orthodontic treatment may be needed.
Maintaining Your Results
After your treatment is complete, maintaining the results is crucial. Retainers are often recommended to prevent teeth from shifting back into their previous positions. Our Worthing orthodontists will provide you with a custom retainer and guidance on how to wear it effectively.
Why Choose Our Worthing Orthodontic Clinic?
Choosing the right orthodontic provider is essential for achieving the best results. Here’s why patients trust us:
- Expertise & Experience – Our team has years of experience in orthodontic treatments.
- State-of-the-Art Technology – We use the latest equipment to provide precise and effective treatments.
- Personalised Care – Each patient receives a tailored treatment plan to ensure the best possible outcome.
- Convenient Location in Worthing – Our clinic is easily accessible to residents in Worthing and the surrounding areas.
- Free Orthodontic Consultations – We offer complimentary consultations so you can explore your options without commitment.
Start Your Orthodontic Journey in Worthing
If you’re looking for professional orthodontic treatment in Worthing, West Sussex, our experienced team is ready to help you achieve a confident, gap-free smile. We offer free orthodontic consultations, allowing you to explore your treatment options and receive a personalised plan tailored to your needs.
Contact us today at Clinic for Implant & Orthodontic Dentistry in Worthing to schedule your appointment. Let’s transform your smile together!
📞 Call us at: 01903-821822
🌍 Visit our website: dental-worthing.co.uk
📍 Location: 7 Chapel Road, Worthing, West Sussex, BN11 1EG
Dental implants in patients affected by systemic diseases - By Dr Amir Mostofi -DDS, Dip. (Ortho.), MSc(Implant.)
Navigating the intricate landscape of dental implantology amidst systemic diseases demands a nuanced understanding and approach. The comprehensive review by Donos and Calciolari delves deep into how systemic health conditions and their associated medications influence the success of dental implants. It highlights the paramount importance of meticulous patient selection, informed by a thorough medical history and the complexity of the surgical site. This narrative is not just about the challenges; it offers a beacon of guidance with practical suggestions for clinicians, aiming to mitigate risks and optimise outcomes. It also casts a spotlight on the need for further research to refine our understanding of these interactions. This exploration serves as a crucial resource for dental professionals, ensuring they are well-equipped to provide care that combines the dual goals of patient safety and implant success.
Dental implants in patients affected by systemic diseases
The exploration of dental implant success among patients burdened by systemic diseases reveals a realm of nuanced considerations, pivotal for optimising patient care and outcomes. Authored by N. Donos and E. Calciolari and published in the British Dental Journal in 2014, this comprehensive review sheds light on the intersection between systemic health conditions and dental implantology, presenting an invaluable resource for dental professionals worldwide.
Systemic diseases, encompassing a wide array of health conditions, often necessitate medications that could influence or complicate the process of dental implant surgery. Understanding the intricate relationship between these systemic conditions and dental implant success is crucial for clinicians, as it aids in the meticulous planning and execution of implant surgeries, ensuring both the safety and well-being of patients. This narrative delves into the evidence surrounding implant survival and success in patients with systemic diseases, offering practical suggestions for clinicians and highlighting areas necessitating further research.
Dental implants represent a cornerstone in the treatment of edentulism, showcasing high survival rates and offering a semblance of natural dentition. The essence of achieving successful implant outcomes lies in judicious patient selection, entailing a thorough medical history evaluation and a comprehensive assessment of the surgical site's complexity. Certain systemic conditions, underscored by varying levels of evidence, have been identified as potential complicating factors or even contraindications to implant surgery. This increasing prevalence of medically compromised individuals seeking dental implants underscores the importance of understanding the impact of systemic diseases and associated medications on both the surgical procedure and the overall treatment outcome.
Among the systemic conditions deemed as absolute contraindications for implant surgery are recent cardiovascular events, recent major surgeries such as valvular prosthesis placement or organ transplants, heightened risk of bleeding, significant immunosuppression, active cancer treatment, and intravenous bisphosphonate therapy. These conditions pose not only a heightened risk of implant failure but also potential grave risks to the patient's overall health.
The review further explores the effect of various systemic diseases on dental implant outcomes, with a focus on bone diseases such as osteoporosis, medication-related osteonecrosis of the jaws (MRONJ), and other less common bone conditions. Osteoporosis, a prevalent bone disease, poses biological plausibility for impaired bone healing around implants, though evidence remains controversial. Antiresorptive medications, particularly bisphosphonates and denosumab, present a risk for MRONJ, influencing implant success rates and necessitating careful patient management.
Diabetes mellitus, characterised by hyperglycemia, has been shown to negatively impact bone metabolism and may impede osseointegration and implant success. The review emphasises the importance of glycaemic control in diabetic patients undergoing implant therapy, alongside the management of other complications associated with diabetes.
Cardiovascular diseases, bleeding disorders, and specific mucosal diseases such as oral lichen planus and ectodermal dysplasia are also scrutinized for their potential impact on dental implant outcomes. The review suggests tailored approaches and precautionary measures for patients with these conditions, aiming to maximise implant success while minimising risks.
The document culminates in general clinical recommendations, underscoring the limited evidence base concerning the effect of systemic diseases on dental implant success. It calls for larger prospective studies to enhance understanding and provide more definitive guidance. Despite a few conditions being labelled as absolute contraindications, the review advises dental professionals to weigh the benefits and risks of implant therapy carefully, engage in interdisciplinary communication, and adopt stringent follow-up regimens for patients with systemic diseases.
In essence, the review by Donos and Calciolari serves as a testament to the complexity of dental implantology within the context of systemic health. It beckons a holistic approach to patient care, emphasising the need for ongoing research, clinical prudence, and a deep understanding of the interplay between systemic diseases and dental implant outcomes.
Understanding Dental Bone Grafts: A Comprehensive Guide - By Dr Amir Mostofi DDS , Dip (Ortho.), MSc (Implant.)
Dental bone grafts are essential procedures for restoring jawbone structure and are crucial for dental implants and overall oral health. They involve adding bone material to the jaw, aiding in bone regeneration, and providing a stable foundation for future dental work.
Understanding Dental Bone Grafts: A Comprehensive Guide
Dental bone grafting is a crucial procedure for patients experiencing jawbone loss, which can significantly impact oral health and the success of dental implants. It involves adding bone material to the jaw, which can be sourced from various origins such as the patient's own body, human or animal tissue banks, or synthetic materials. This procedure acts as a scaffold, allowing the patient's own bone tissue to grow and regenerate. Dental bone grafts are often essential for individuals who have lost teeth, are planning dental implant surgery, require dentures, or have suffered bone loss due to gum disease.
Types of Dental Bone Grafts
There are several types of dental bone grafts, each serving a unique purpose:
Socket Preservation: Performed immediately after tooth extraction to prevent socket collapse.
Ridge Augmentation: Enhances the jawbone's width and volume, particularly after long-term tooth loss.
Sinus Lift: Elevates the maxillary sinuses to allow for implant placement in the upper jaw.
Periodontal Bone Graft: Targets bone loss caused by gum disease, providing stability to loose teeth.
Procedure Details
Before the Procedure The process begins with a thorough oral examination and dental imaging to assess bone loss. Based on these findings, a personalized treatment plan is developed.
During the Procedure The procedure involves administering local anesthesia, making a small incision in the gums, and placing the bone graft material in the required area. A membrane may cover the graft for added protection. Finally, the incision is closed with stitches.
After the Procedure Post-surgery, patients might experience pain, swelling, and bruising, which are manageable with pain relievers and possibly antibiotics. It's normal to find small bone fragments in the surgical area during initial healing.
Pain and Sedation Dental bone grafts are generally low in pain. Sedation options vary, from local anesthesia to general anesthesia, depending on the case complexity.
Success and Failure The success rate of dental bone grafts is high, but smoking or certain medical conditions can increase the risk of failure. Warning signs include worsening pain, pus, gum recession, and lack of jawbone improvement.
Risks and Benefits
While generally safe, potential risks include infection, bleeding, nerve damage, and anesthesia complications. The benefits include increased eligibility for dental implants and restoration of jaw structure.
Recovery and Outlook
Recovery varies, typically taking three to nine months for complete healing. Most people can resume normal activities the day after surgery.
When to Contact Healthcare Providers
Patients should watch for severe pain, increased swelling, pus around the grafting site, or fever and contact their dentist if these occur.
Summary
Dental bone grafts are vital for restoring oral health and function in individuals with jawbone loss. They play a critical role in preparing for dental implants and combating the effects of tooth loss and gum disease.
Navigating the Misconceptions: Bone Grafting and All on 4 Dental Implants- By Dr Amir Mostofi DDS, Dip. MSc
The All on 4 dental implant technique is transforming full jaw restoration, challenging long-held beliefs about bone grafting. Traditionally, dental implants often required bone grafting to compensate for insufficient bone volume. However, All on 4 implants frequently bypass this necessity due to their unique design and placement strategy. This innovative method involves positioning four implants in the jaw, utilizing existing bone structure, even where volume is limited. The success of this procedure, especially without bone grafting, heavily relies on the dentist's skill and precision. Experienced professionals adept in implantology can effectively leverage the jaw's anatomy, reducing the need for additional invasive procedures. Avoiding bone grafting offers numerous advantages, including shorter treatment times, less invasive surgery, and faster recovery. This approach not only enhances patient comfort but also immediately improves dental functionality and aesthetics.
Navigating the Misconceptions: Bone Grafting and All on 4 Dental Implants.
By Dr Amir Mostofi DDS, Dip. MSc
The realm of dental implant technology has witnessed significant advancements in recent years, with All on 4 dental implants emerging as a pivotal solution for full jaw rehabilitation. This revolutionary technique has not only enhanced the efficiency of dental restorations but has also challenged common perceptions, particularly regarding the necessity of bone grafting.
Understanding All on 4 Dental Implants:
All on 4 dental implants offer a comprehensive solution for patients with significant tooth loss. This procedure involves the strategic placement of four implants in the upper or lower jaw, providing a stable foundation for a full-arch prosthesis. The technique is celebrated for its minimally invasive nature and its ability to deliver immediate results.
Debunking Bone Grafting Myths in All on 4 Implants:
Contrary to popular belief, All on 4 dental implants often do not require bone grafting. This misconception stems from traditional implant procedures where insufficient bone volume necessitated grafting. However, the innovative design and strategic placement of All on 4 implants typically bypass the need for such additional procedures.
The Science Behind No-Bone-Grafting in All on 4 Implants:
The key lies in the angulation and placement of the implants. By tilting the posterior implants, All on 4 takes advantage of the existing bone structure, even in cases where bone volume is limited, thereby eliminating the need for grafting in many instances.
Expertise Matters: The Role of Skilled Dental Professionals:
The success of All on 4 implants without bone grafting hinges on the expertise of the dental professional. Precision in implant placement is crucial, requiring an in-depth understanding of oral anatomy and advanced surgical skills. This expertise ensures optimal use of available bone and minimizes the need for grafting.
Advantages of Avoiding Bone Grafting:
Avoiding bone grafting in All on 4 procedures offers several benefits:
Reduced treatment time
Less invasive surgery
Lower risk of complications
Quicker recovery and healing
Immediate improvement in functionality and aesthetics
Conclusion
All on 4 dental implants represent a significant leap forward in oral rehabilitation. By potentially eliminating the need for bone grafting, they offer a quicker, less invasive, and more efficient solution for full jaw restoration. However, the key to success lies in the hands of skilled dental professionals whose expertise can make a significant difference in the outcome. As with any medical procedure, it's essential for patients to consult with experienced dental practitioners to explore the best options for their specific needs.
Creating Perfect Dentures at Home with a Dentist Who Comes to You- By Dr Amir Mostofi DDS Dip MSc
Creating custom dentures at home with the expertise of a domiciliary dentist is an ideal solution, especially for patients facing unique challenges. Clinic for Implant & Orthodontic Dentistry prioritises patient-centred care, ensuring the utmost comfort and satisfaction throughout the process. Our journey begins with a comprehensive initial consultation, followed by extractions if necessary. Accurate impressions of your jaw are taken, even in cases of shrinking jawbones. We provide flexibility, allowing alterations during the wax trial denture stage at no extra cost. For those with cobalt chrome dentures, we handle the challenges seamlessly. We also offer domiciliary dental care for home-bound or bed-bound patients, ensuring safety and convenience. Our goal is to craft dentures that restore your smile and improve your quality of life.
Creating Perfect Dentures at Home with a Dentist Who Comes to You
Dentures made in the convenience of one's own home with the assistance of a domiciliary dentist are an excellent option for those who find traditional dental visits difficult. At Clinic for Implant & Orthodontic Dentistry, we specialise in providing denture services that are tailored to the specific requirements of our patients, including those with dementia and other mental disorders. In this exhaustive guide, we will walk you through the various phases of denture creation, from initial consultations to the final fitting, while emphasising the significance of a domiciliary dentist's experience in managing complex cases.
Step 1: Consultations at the outset
The initial consultation is a crucial first stage in the process of acquiring dentures. During this appointment, our domiciliary dentist conducts a comprehensive examination of your oral health and discusses the denture options that best meet your requirements. For a number of our patients, particularly those with dementia, collecting impressions can be difficult. Our experienced domiciliary dentists play a crucial role in the management of such cases. During this phase, we also ensure that all necessary documentation, including consent forms and cost discussions, is completed.
Step 2: Extraction, if Required
When oral health issues are identified during the initial consultation, tooth extraction may be required. To minimise patient distress, tooth extraction is performed with care and frequently in stages. This period, which typically lasts between one and three weeks, allows the mouth to recuperate and reduces swelling, making future dentures fit better.
Step 3: Taking Impressions
Taking accurate impressions of your upper and lower mandible is a crucial step in the fabrication of dentures that fit securely and comfortably. Numerous elderly individuals struggle with thinning jawbones, necessitating the use of specialised impression-taking techniques. Our domiciliary dentists are well-versed in adapting these techniques to individual requirements, thereby ensuring an accurate representation of your mandible and any remaining teeth.
Step 4: Registration of the Bite
At the stage of bite registration, the complex relationship between your upper and lower mandible is established. This procedure enables the dentist to record the precise relationship between your jaws. In addition, during this phase, the colour, shape, size, and quality of the denture teeth are meticulously determined, ensuring that your dentures appear and feel natural.
Step 5: Wax trial dentures
Seeing the wax trial dentures in your mouth is a crucial step in the process of creating dentures. This phase enables both you and the dental technician to evaluate whether the desired aesthetic has been achieved. At this juncture, any necessary modifications can be discussed and implemented. At Clinic for Implant & Orthodontic Dentistry, we prioritise your satisfaction, and alterations are made at no additional cost if necessary.
Step 6: Final Fitting and Adjustments
In the final stage, the completed dentures are adjusted. If significant changes were made during the wax trial denture stage, it may be necessary to repeat appointment 4. We recognise that the process of having dentures fitted can be intimidating, especially for first-timers or those who have had negative experiences in the past. Our dedication to ensuring that you comprehend the procedure and our emphasis on both form and function ensure that you leave with dentures that inspire confidence.
Visits and Problems with Cobalt Chrome Dentures
Generally, between four and seven visits are required to complete a denture, depending on the individual's requirements and complexity. However, cobalt chromium dentures, which contain a metal skeleton, typically require more visits due to the complexity of their fabrication and adjustment. Our skilled team at Clinic for Implant & Orthodontic Dentistry is well-equipped to handle such challenges, assuring the best possible outcome for your cobalt chrome dentures.
Domiciliary dental care for patients confined to their homes or beds
We recognise that not all patients have easy access to dental clinics. For this reason, we offer home visits, also known as domiciliary dental care, to those who are bedridden or confined to their homes. We make the process as convenient and comfortable as possible for patients who can recline in a wheelchair or regular chair with space around the dentist's workspace.
If a patient is completely bedridden and inclining the bed is not an option, we do have a solution. We use intraoral digital scanners as opposed to traditional impression materials, thereby eliminating the danger of material running down the patient's throat and ensuring a safe and efficient procedure.
The conclusion
A personalised and patient-centered approach to dental treatment is the fabrication of dentures in the patient's residence by a domiciliary dentist. At the Clinic for Implant & Orthodontic Dentistry, we strive to make this journey as pleasant and rewarding as possible, particularly for patients confronting unique obstacles. We have the knowledge and skill to create dentures that restore your smile and improve your quality of life. If you would like to schedule an initial consultation, please contact us at 01903-821822. We anticipate serving you and ensuring that your dental requirements are met with the utmost care and expertise.
Top 5 Sources of Dental Implant Pain When "There's Nothing Wrong with the Implant"- By Dr Amir Mostofi, DDs Dip MSc
Experiencing pain after a dental implant, even when everything looks fine? Explore the top 5 reasons behind post-implant discomfort and find solutions to ensure a comfortable journey towards a perfect smile.
If you've recently had a dental implant and are experiencing pain even though everything seems normal, you're not alone. This article aims to explain the top 5 reasons behind dental implant pain when there's no apparent issue with the implant itself, in a way that's easy for patients to understand.
1. Violations of the Inferior Alveolar Canal (IAC):
The IAC is a canal that houses the inferior alveolar nerve (IAN), which plays a crucial role in sensation for your lower jaw. Sometimes, the IAN takes a unique path, forming what's called an "anterior loop." Trauma to this area during implant placement can lead to sensory disturbances, bleeding, and pain. Recent research suggests that getting closer to the IAC may not be as risky as previously thought, as long as the nerve isn't directly affected.
2. Violations of Branches in the Mandibular Canal:
Traditionally, we've considered the IAC as a single canal to be avoided during implant surgery. However, it's now known that smaller branches can exist alongside the main canal, creating a network. If these branches are accidentally disturbed during surgery, it can result in pain. These branches are often missed because they aren't widely recognized, but they can show up on X-rays or CT scans.
3. Inadequate Keratinized Tissue:
Keratinized tissue is the protective, tough tissue that surrounds your implant crown. Some studies suggest that not having enough of this tissue (usually at least 2 mm wide) can lead to pain, especially when you touch or use the implant, like when brushing or eating. Fortunately, this issue can often be resolved by adding more tissue through a soft-tissue graft.
4. Poor Bone-to-Implant Contact:
Even if an implant looks fine on X-rays and CT scans, it's possible that the bone around it isn't providing a secure foundation. This can happen when fibrous tissue forms around the implant instead of sturdy bone. This may not be visible in regular exams, but patients can still feel pain when using their implant, especially when it's fitted with a crown. A resonance frequency analysis machine can help diagnose this issue by measuring the strength of the implant-bone connection.
5. Predisposing Risk Factors:
Sometimes, pain after implant surgery can be linked to factors that exist within your medical or genetic makeup. Conditions like fibromyalgia, temporomandibular disorders, and depression/anxiety can make you more prone to experiencing pain. This type of unexplained pain often falls under the category of "peripheral painful traumatic trigeminal neuropathy" (PPTTN).
In summary, if you're feeling pain after a dental implant, even when everything looks fine, it's important to consider these factors before assuming it's psychosomatic. There are various reasons behind implant-related pain, and a thorough evaluation is essential to pinpoint the cause accurately. Your dental professional can help you identify and address the issue, ensuring your dental implant journey is as comfortable as possible.
A Clinic for Root Canal Treatment Near You
The prospect of a first-time root canal can be daunting, but it offers a relatively quick and virtually painless solution when standard fillings can't save a tooth. Severe tooth pain, sensitivity, discoloration, and other symptoms may indicate the need for a root canal. The procedure involves local anesthesia, cleaning, and filling the tooth's root canal. While root canals have an unfair reputation for pain, most discomfort subsides within 72 hours. Costs vary but can prevent the need for extractions. Success rates are high at approximately 95%, with proper post-treatment care. Myths about pain, cost, and recovery often overshadow the benefits of this essential dental procedure.
The prospect of undergoing a root canal for the first time can be intimidating. In situations where a standard filling cannot save the tooth, a root canal can provide a relatively quick and painless solution.
Regarding Root Canal
Do I require a root canal procedure or endodontic treatment?
If you are experiencing severe tooth pain, extreme sensitivity, tooth discoloration, swollen gums, a recurring abscess on the gum line, or a fissure in a filling, or if you have sustained a traumatic injury to your teeth, you may require a root canal to save your tooth. If your dentist believes you are likely to need a root canal, they will take an X-ray and may test for temperature sensitivity; they may also perform comprehensive imaging. If you have an abscess, your dentist may prescribe antibiotics to treat the infection before commencing treatment, or he or she may recommend a root canal.
If I require a root canal, what is the next step?
It is essential that you comprehend the root canal procedure, the risks and benefits of the treatment, as well as the treatment's complexity. Root canal treatments are now specially registered with the GDC, and in some cases, your dentist may advise you that a referral to a dentist with a special interest in root canals or endodontics is necessary to ensure long-term success and provide the most effective treatment. Local anaesthesia will be administered to ensure that your root canal treatment is painless. A rubber dam will be inserted around the tooth to maintain a dry environment. An access hole will be drilled, and then decayed nerves and detritus will be removed with files. Then, the root canal will be filled with a polymer compound. Then, a temporary filling may be placed, or in some cases, the permanent filling may be completed at the same appointment.
My root canal treatment will be painful?
Root canal treatment has an unjust reputation for being painful, primarily because patients typically discover they need one after experiencing excruciating tooth or gum pain. As local anaesthetic will be used throughout your treatment, you will experience minimal discomfort at most. 24–72 hours of soreness and discomfort are common following endodontic treatment.
How much does the treatment of a root canal cost?
For the price of a root canal, please visit our website's fee page HERE. In many cases, a root canal can prevent the need for an extraction, and if you take good care of your teeth and tissues after the procedure, root canal treatment can last a lifetime with routine maintenance and check-ups. Please note that following a root canal, you will need a restoration such as a filling or crown. In addition to the cost of root canal, the cost of a filling or crown will be added.
What is the rate of success for root canals?
95% approximately. In extremely uncommon instances, we may discover additional infection in the root after performing a root canal and need to administer additional treatment. In extremely rare circumstances, a root canal may not be able to save the tooth. However, as a treatment with a success rate of 95% and durability for the majority of patients, a root canal is typically an excellent method to avoid extraction. Our opinion is that root canals should be performed by a practitioner with postgraduate experience in this discipline. Treatments and technologies have progressed, increasing the success rate of root canals.
What should I do after the treatment of my root canal?
After your treatment, you may desire to take an over-the-counter pain reliever, such as Aspirin or Ibuprofen, for minor pain or sensitivity. Ensure that you finish any antibiotics prescribed by your dentist and that you continue to brush and floss as usual. Long-term vigilance with brushing and flossing is essential for maximising the effectiveness of root canal therapy. If properly maintained, a root canal can last a lifetime. In the past, patients were typically told that a root canal would last between 8 and 10 years, but we'd add that the longer you want your root canal to last, the better you must care for your teeth and gums! Not smoking, flossing and scrubbing your teeth religiously, and visiting your dentist and hygienist on a regular basis will all contribute to the longevity of your root canal. According to research, all post-root canal procedures should include a crown inlay and post.
Is a root canal a very long procedure?
Root canal procedures can take between two and three hours, depending on their complexity. We may be able to complete your root canal in a single appointment, which will take approximately 90 minutes, but root canals are technically challenging, so time must be taken to achieve the best results.
What are the most prevalent root canal treatment myths?
Root canals are an excruciating procedure. Yes, if you require a root canal, you may arrive at the clinic in agony, but this should subside once we begin treatment! Patients frequently report that the relief they experience once root canal therapy begins and we can stop the tooth and gum pain they've been experiencing is immense, and that root canal therapy itself should be painless.
The cost of root canals is high. They are more expensive than standard composite fillings, but significantly less expensive than dental implants, and if you detect your dental issues early, a root canal may prevent you from needing an implant in the future. A naturally saved root canal is always preferable to an implant, and while the prospect of spending up to three hours in the dentist's chair may be daunting, it's worth it to be pain-free and save your tooth!
That root canals are time-consuming. We may be able to complete your root canal treatment in a single visit, but even if it requires multiple visits, it's a surprisingly quick and effective method to save your tooth!
Root canals have a lengthy recovery period. Similar to after having a filling, you may experience some sensitivity, but this should subside within two days. Additionally, we recommend biting a little more gently on the treated tooth for the next day or so, and Ibuprofen can be consumed. Aside from this, there is virtually no recovery period following a root canal. Just be sure to brush and floss thoroughly, and business as usual will resume after your procedure.
That root canals are not durable. We will provide you with the highest conceivable standard of care. Then the floor is yours. If you take good care of your teeth after root canal therapy, root canals can last for many years. Like anything else, root canal treatment may appear to be costly, time-consuming, and intimidating, but if performed by the right practitioner with the right experience, root canal treatment should be pleasurable and successful!
All There to Know About Dental Implants: A Patient Guide
A dental implant is an artificial tooth root that is typically composed of titanium. When applied with skill, they provide a highly reliable treatment. The primary objective of implant placement is to obtain immediate, intimate contact with the surrounding bone. Over time, additional bone growth on the implant surface improves the implant's stability.
All There Is to Know About Dental Implants : A patient guide
In modern dentistry, dental implants have become the treatment of option for missing teeth.
What exactly is an implant?
A dental implant is an artificial tooth root that is typically composed of titanium. When applied with skill, they provide a highly reliable treatment. The primary objective of implant placement is to obtain immediate, intimate contact with the surrounding bone. Over time, additional bone growth on the implant surface improves the implant's stability.
In order to support replacement teeth, dental implants typically feature an internal screw thread or post space that permits the attachment of a variety of components. Once in place, these components provide long-lasting support for crowns, bridges, or removable dentures.
Who can receive dental implants?
Dental implants are appropriate for the majority of healthy adults. They can only be used once the jawbone has ceased growing, so they are typically not used on children. Habits such as excessive drinking or smoking can increase the number of complications associated with initial healing and may be detrimental to the gum and bone surrounding each implant in the long term. Smoking should be reduced or best still given up altogether. However, each case is unique, and if you have any medical issues, you should consult with one of our implant specialists prior to beginning treatment; in only a few instances do health issues completely preclude the use of dental implants.
Dental implants are appropriate for the majority of healthy adults.
How will you determine if you are a candidate for implants?
During your initial consultation, one of our specialist will determine whether implant treatment is feasible. We discuss your options and conduct an examination of your mouth and remaining teeth to determine the nature and extent of any existing dental issues. Typically, x-rays will be obtained and dental models will be fabricated so that these can be examined after your appointment. These x-rays and models will be used to determine the optimal position for an implant, the number of implants required to fill the gap, and the available bone grade and volume.
Establishing excellent oral hygiene is a crucial step in any treatment plan. At this initial consultation, you will be informed of which problems are essential and what treatment is necessary to stabilise any gum or tooth issues.
Must you maintain a wholesome mouth?
When you inquire about dental implants for the first time, it is frequently in response to ongoing dental issues or the recent loss of teeth. Before implant treatment, it will often be necessary to understand and treat the underlying cause of these issues.
If you have poor breath, loose teeth, or excessive bleeding, especially when your teeth are professionally cleaned, you may have gum disease.
Gum disease (periodontal disease) is a leading cause of bone loss, making dental implant treatment more difficult, but not impossible.
How lengthy is the treatment?
For routine cases, the duration between implant placement and the placement of the first tooth/teeth can range from three to six months. The availability of higher-quality bone can be used to reduce treatment time, whereas inferior bone requires more time and care, which can extend treatment times beyond six months.
What should you understand before beginning treatment?
You will receive a written summary of your discussion regarding treatment planning, emphasising your current dental condition and any alternatives to dental implants. This summary also provides an overview of the anticipated treatment stages and provides an estimate of the expected duration, number of implants, and cost. There may be additional issues unique to your case, and they will be addressed accordingly.
How long do implants typically last?
Once the implants and surrounding soft tissues are deemed to be healthy and the new teeth are deemed to be comfortable and properly aligned, the quality of your oral hygiene and willingness to attend regular maintenance reviews will have the greatest impact on their longevity.
Similar to neglected natural teeth, implants will develop a layer of hard and porous deposits (calculus and plaque) if they are not properly cared for. These deposits, if left untreated, can cause gingival infection, bleeding, soreness, and general discomfort. Implants could be said to have the same longevity as natural teeth. Implants that are well-maintained and placed in sufficient bone can potentially last a lifetime if cared for properly. However, just as you would anticipate traditional crowns, bridges, and fillings to require occasional restorations or replacements, implant-supported teeth may also require similar maintenance over time.
How many teeth can dental implants support?
Dental implants can be used to replace a single tooth or an entire arch of teeth. Dental implants can support all prevalent forms of tooth replacement, such as bridges and dentures.
If you are missing a single natural tooth, one implant will typically suffice to provide a replacement. However, larger spaces created by two, three, or more missing teeth may not require one implant per tooth; the precise number of implants will depend on the grade and quantity of bone at each potential implant site.
Patients with a propensity of clenching or grinding their teeth (bruxism) may be at risk of implant overload. Bruxism occurs during sleep for most individuals, so they are typically unaware of it. The most common clinical indications of bruxism are excessively worn or flattened teeth, chipped enamel edges, and/or the frequent breakage of filling fragments. During treatment planning, the effects of bruxism must be considered, and they can be compensated for by placing additional implants, selecting appropriate restorative materials, and providing a nighttime bite guard to secure the new teeth. This will be covered in your initial consultation and treatment plan.
Implant retained prostheses
What is the therapy?
Using dental implants to anchor removable prostheses is a significantly more effective method than using adhesives, pastes, or powders. With only two implants or four mini implants in each jaw, dentures can be clipped into position and held securely, but are simple to remove for cleaning and sleeping. Implants also provide a number of aesthetic advantages, including the preservation of bone in the jaw and the maintenance of facial structure, as well as the restoration of lost lip support to reduce wrinkles around the mouth. Approximately 15 minutes of the 90-minute procedure are devoted to actual surgery. It is a quick and economical alternative to a complete arch of dental implants.
What alternative treatments are available?
Implant-retained dentures are a significant improvement over traditional removable dentures, which are inconvenient, sometimes uncomfortable, and restrict your diet. Full arch dental implants are an even better alternative to removable dentures; we are one of the few practises in East Anglia with the expertise to conduct this procedure. It's a life-altering, permanent solution.
Is it essential to replace an entire set of lacking teeth?
Multiple tooth loss can have a profound effect on one's quality of life. In addition to having a significant influence on your ability to speak and eat, it can also alter your appearance. Without teeth to support the lips and cheekbones, wrinkles develop more quickly and the cheeks become hollow. Many individuals with this type of tooth loss believe they appear older than they are, which can be detrimental to their self-esteem.
A summary of the implant procedure
Typically, implant treatment consists of several phases that occur over a period of three to nine months. Although there are numerous implant treatment methods, a typical procedure typically involves the following:
Assessment and planning for treatment:
At the initial consultation, after a thorough discussion of all potential alternatives, we will determine whether implant treatment is feasible. If necessary, x-rays will be obtained and models of the teeth will be created. Then, a written treatment plan detailing the treatment sequence and associated costs will be created.
Implant placement:
Implant implantation is a relatively straightforward minor surgical procedure that can be performed in a dental office under sterile conditions.The procedure is performed under local anaesthesia and, if necessary, sedation. If, during evaluation, it is determined that the underlying bone is deficient, there are several options for bone regeneration. Depending on the needs, bone regeneration is typically performed at the same time as implant placement.
Transition period:
It can take between six weeks and six months for implants to integrate with a patient's bone. During this period of integration, temporary dentures or bridgework may be worn as needed. In certain instances, temporary teeth can be affixed to the implants in a procedure known as "immediate loading" while the implants integrate.
The Recuperative stage:
Once implants are incorporated, they can be restored with a variety of new teeth (definitive restorations) including a single crown, small or large bridge, or removable overdenture. We collaborate closely with a laboratory that creates these permanent restorations.
Maintenance:
Following conclusion of implant treatment, the patient must clean the new teeth (restorations) according to the instructions. A dental hygienist may also provide guidance on the care and upkeep of restorations and natural teeth. Regular visits to the dentist are required so that the health of the soft tissues, bone levels, and restoration can be evaluated.
How can you determine if you have sufficient bone for dental implants? Normal dental x-rays display a great deal of detail, but only in two dimensions. From these views, it is typically possible to determine the height of available bone for implant placement; however, sometimes more advanced imaging techniques are required to determine the equally crucial bone breadth.
Dental CBCT Scans – there are now a number of sophisticated x-ray techniques that enable a three-dimensional examination of the jawbone. CBCT (cone beam computed tomography) scans are the most precise and widely available. Images obtained by CBCT scanning will typically display all of the necessary bone information, including quantity and quality, but most importantly the presence of structures that must be avoided.
What may result in bone loss?
When a tooth is lost or extracted, a significant portion of the bone that once encompassed the remaining root may be lost. This loss is referred to as "bone resorption" and can be especially rapid during the first few months. Despite the fact that the rate and quantity of bone resorption is highly variable between individuals, it will always occur to some degree unless special precautions are taken to mitigate its effects.
Many patients report that their dentures gradually become looser and no longer fit as well as they once did. Initially, the observed worsening of denture fit is a result of the increased rate of bone loss following tooth extractions.It is the direct effect of gnawing forces that causes the gradual deterioration of supporting bone over time. Therefore, the longer prostheses are worn, the less available bone there is for dental implants.
What anatomical structures must be avoided during dental implant placement?
As long as the implants remain within the bone that once supported your natural teeth, there are no significant risk areas in the upper mandible. If you are missing upper back teeth, you can be shown the contour and location of the area above the roots (maxillary sinuses). Since the maxillary sinuses are visible on the majority of x-rays, they are generally avoided.
The 'inferior dental nerve' is the most vital anatomical structure to avoid in the lower mandible. This nerve begins behind the wisdom teeth, travels under the back teeth (molars), and emerges on the epidermis of the face where the middle teeth (premolars) are or were. This is the reason why a normal dental anaesthetic numbs the lip even when the needle is inserted in the very back of the mouth. If this nerve is irritated or damaged during dental implant implantation, it can result in temporary or permanent numbness or altered sensation. This is an uncommon but significant complication.CBCT scans are typically the most accurate method for pinpointing the location of this nerve, allowing implants to be implanted with confidence. CBCT scans are more expensive than standard dental x-rays, but the information they provide is often invaluable for complex treatment planning and determining the location of vital anatomical structures. If a tooth is inadvertently damaged by the implantation of a nearby implant, any resulting issues can typically be treated with root canal therapy, in which the tooth's nerve is removed.
Can dental implants preserve bone?
This is one of the most essential characteristics of dental implants. Once in place and supporting teeth, daily functional forces (eating, smiling, speaking) stimulate the adjacent bone, causing it to become denser and stronger. As with all things, there are limitations to the amount of labour an implant can perform. We will discuss this in greater depth as it pertains to your specific situation.
Can replacement teeth be worn while undergoing implant treatment?
If the teeth being replaced by dental implants are in a highly visible area of the mouth, it is probable that you will need to have some teeth present during the procedure. This can be accomplished in a variety of methods, ranging from simple plastic dentures to removable bridges. If replacement teeth are used during treatment phases, it is vital that they do not exert uncontrolled pressure on the implants. You should anticipate a number of visits for minor adjustments to any temporary teeth after the implants are inserted and before they are activated. They might not be as visually appealing as your final restoration.
Are dental implants compatible with natural teeth?
Dental implants are routinely inserted adjacent to natural teeth, and this procedure is generally very safe. The only exception to this rule would be if the natural root was extremely curved or inclined in the proposed implant path. This could cause the implant to damage the root, but this is typically avoidable through meticulous pre-operative planning.
Are the replacement molars fused together?
When numerous implants are inserted, they are typically connected in the same manner as a bridge supported by natural teeth. When teeth supported by implants are joined together, they are mechanically sturdier than the sum of their parts.
If sufficient implants are available, it is frequently simpler and just as effective to construct several smaller bridge sections, each supporting a few teeth. The overall effect in the mouth is identical, and if you ever need to repair one of the minor sections, this can be accomplished much more easily. Again, the quality of the bone, as well as the number and placement of the implants, will determine which option is most suitable for you.
Is it unpleasant when implants are inserted?
The majority of patients will be familiar with the anaesthetics used in routine dentistry and will be aware of their efficacy. The same anaesthesia is used to insert implants. Depending on the complexity of your case, the procedure could last anywhere from 30 minutes for a single implant to several hours for complex bone augmentation and implantation of multiple implants. Expect some minor swelling and occasional discoloration after surgery. For the majority of patients, fundamental over-the-counter pain relievers will suffice for several days. If you continue to experience discomfort, contact your healthcare provider, who can prescribe a stronger medication.
Generally, healing is uncomplicated, and sutures are removed within a week to ten days. During the initial few days, you should disclose any unanticipated pain or swelling so that it can be evaluated. Always seek advice when in doubt, as early detection of a problem often leads to a simplified solution. You may also be prescribed antibiotics and asked to perform some basic procedures, such as rinsing your mouth with salt water or an antiseptic mouth rinse. It is essential that you follow these directions.
If the implant surgery will require a long time, is sedation an option?
Although it is relatively simple to provide effective pain management during surgery, the majority of patients will be apprehensive. There is no need to suffer in silence, as there are numerous highly effective ways to attain a state of relaxation.
Conscious sedation – For more complex procedures, it may be recommended that you have a more regulated method of relaxation and comfort during the surgical phases. This is known as 'conscious sedation' and is distinct from a anaesthetic because you are awake enough to respond to simple instructions that may be helpful to the surgeon; however, you will recall almost nothing of the treatment phase. It is especially advantageous for procedures lasting more than an hour that do not require hospitalisation; this is likely the case for the majority of dental implant treatments.For routine "conscious sedation," a sedative is administered via an arm or hand vein for the duration of the procedure. An anesthesiologist continuously monitors your pulse rate and oxygen levels during this extremely safe procedure. A standard dental local anaesthetic is injected around the proposed implant sites under conscious anaesthesia. By the time the dental anaesthetic is administered, the anaesthesia has already taken effect, so most patients do not recall this phase. For procedures requiring oral or conscious anaesthetic, you may be asked to refrain from eating or drinking for at least four hours prior to surgery, and you will be required to make arrangements for an adult to drive you home. Additionally, you will be instructed not to operate any apparatus for at least 24 to 36 hours.
What can be done if there are insufficient bones?
Up to this point, we have covered the fundamentals of routine implant placement. This has included the initial examination and diagnosis, special x-rays such as CBCT scans, anaesthetic during surgery, and what to expect following the placement of implants. However, for some individuals, bone loss following tooth extraction or loss prevents the placement of an implant. There are actions that can be taken if this occurs:
It is possible to increase the height of available bone in the upper jaw above the back molars by creating new bone in the sinus.This process is known as a "sinus augmentation." Without the widespread success of this technique, numerous patients would be unable to receive dental implants in a region of the mouth where tooth loss is so prevalent.
There are numerous methods for adding bone, but one of the simplest is to remove a piece of bone from another location and attach it as a "onlay graft" to a deficient area. The new piece of bone will gradually fuse with the underlying bone, and an implant can be implanted in a more favourable position once it has healed and matured.
Where can additional bone be obtained?
Bone can be harvested from a variety of locations, but most commonly from the back of the lower mandible or the chin. Occasionally, it is extracted from the hip or tibia. When using your own bone to create new bone in another area of the mandible, you will experience discomfort at both the donor site and the surgical site. As your own bone is typically regarded as the 'gold standard,' many people feel that the additional discomfort is well worth it.
Alternatives to your own bone for augmentation There are other sources of bone, such as bovine (derived from cows), porcine (derived from pigs), and synthetic materials that have been specially processed to make them acceptable for use in humans, for those who prefer an easier but slightly slower solution. All of these materials, including your own bone, are merely scaffolds into which new bone will grow in a few months in preparation for dental implant placement.
It can take anywhere from three to twelve months for new bone to be suitable for dental implants. Do not rush to advance to the next stage. A larger quantity of bone will take longer to mature than a smaller quantity. Each surgeon will have a preferred technique for producing new bone. Many of them will additionally employ a technique known as "guided tissue regeneration." By placing a barrier material between slow-moving bone cells and the fast-moving cells of the soft tissues lining the mouth, this technique allows slower-moving bone cells time to occupy a space. This is a "resorbable barrier" that will dissolve spontaneously after a few months of performing its function.
Does bone augmentation impact treatment duration?
If you require bone augmentation, it may lengthen the duration of your treatment; however, when performed successfully, it will significantly enhance the outcome of the implant(s) placed. When used in the front of the mouth, it can also enable the construction of much more aesthetically pleasing results.
Regardless of the method selected to increase bone density, the time, effort, and expense are generally worthwhile.
How do you care for your implants?
To increase the longevity of your implants, it is imperative that you maintain excellent oral hygiene. Cleaning your implants is straightforward. For the majority of implant-supported teeth, you will be able to brush and floss around each supporting implant just as you would around natural teeth and tooth-supported bridges. Maintaining excellent oral hygiene may require special floss, interdental toothbrushes, and other cleaning aids in some areas.
If you wish to maintain optimal implant health, it is reasonable to anticipate that some daily maintenance procedures will be more complex than those performed around your natural teeth, and that you will need to devote more time than in the past.
During the first few months following implant placement, your dentist may request that you visit them more frequently; however, once they are satisfied that your treatment is proceeding according to plan, your ongoing dental care will be comparable to that of a patient with natural teeth.
What options exist if an implant fails?
The average success rate for dental implants is approximately 96%; you should discuss how the loss of an implant could affect your treatment plan. A dental implant can fail for a variety of reasons, including smoking, poor oral hygiene, and systemic disease. In these particular high-risk groups, one would anticipate a much higher failure rate. If an implant does not integrate well with the surrounding bone, it will ultimately lose its ability to support replacement teeth and become loose. Commonly, a failing implant does not cause discomfort, and if there are sufficient residual implants, it may not be necessary to replace it.
It is essential to discuss the potential complications that may arise.
Various implant procedures
One-stage implant – The implant is inserted into a fresh, healing, or healed extraction site where the original tooth was extracted, and is immediately visible above the gum. This technique has the advantage of not requiring a second surgical stage to expose the implant. Typically, the implant will not be able to sustain a tooth for several weeks or months.
This is the first stage of a two-stage implant, in which the implant is inserted into a fresh, healing, or healed extraction site and then concealed by a layer of gum tissue. At the second stage, weeks or months later, the implant is uncovered and components are added, bringing it to the surface of the gum so that a new tooth can be attached.
Same-day implants necessitate meticulous planning prior to the actual day of surgery. A few hours after the placement of multiple implants, a full arch of temporary or permanent teeth can be affixed. If temporary dentures are used, they are typically replaced with a permanent bridge after a sufficient period of healing. Not all patients are appropriate candidates for this method of treatment.
In this procedure, a tooth is extracted and an implant is placed promptly into the extraction site. Depending on the local bone and soft tissue conditions, implant surgery may be performed in one or two stages. Not all patients are candidates for this treatment.
Immediate implant placement and early loading – This is dissimilar to immediate implant placement. It is essentially a one-step procedure in which the implant is inserted into a fresh, healing, or healed extraction site and a replacement tooth is attached at the same appointment. This first tooth will typically be kept out of direct contact with opposing teeth for more than three months, following which it will be restored. This procedure is more prevalent in areas of the mouth where aesthetics play an essential role. Again, this approach is not suitable for all patients.
Frequently asked questions:
Will I be able to consume my favourite foods afterwards?
Patients should be able to consume a normal, nutritious diet with little to no difficulty upon completion.
What are the costs associated with implant treatments?
The price can vary based on the required level and extent of treatment. A written treatment plan therefore explains and confirms the total cost.
How much time will it take?
Implant treatment typically requires multiple appointments over the course of several months. In certain instances, implant procedure can be completed much more quickly.
How lengthy is its duration?
Regular dental hygiene and regular checkups should ensure that implants last for many years after treatment is complete.
Am I too elderly to receive implants?
There is no upper age limit for patients undergoing implant treatment, so long as they remain in reasonable health.
Is the procedure painful?
Patients are frequently astonished by the lack of pain they experience during and after implant procedures.
Glossary:
-Abutment
Abutment is the component that connects the implant to the permanent tooth restoration.
-Barrier membrane
A membrane that is draped over a bone defect or bone implant to prevent the infiltration of soft tissue, which could compromise the healing process.
-Bone augmentation
This is the insertion of natural or synthetic bone material in a deficient area of natural bone. This procedure may be performed concurrently with implant implantation, or as a separate procedure prior to implant placement.
-Bone resorption
Resorption of bone is the loss of bone height and/or width in the upper or lower mandible. This process continues throughout life, but is accelerated in areas where teeth have been lost.
-Bridge
A bridge is a method for replacing one or more missing teeth with artificial teeth that are bonded to adjacent natural teeth or dental implants. Bridges may be glued in position (adhesive bridges) or supported by crown preparations (conventional bridges) and constructed from a number of different materials.
-Bruxism
The act of clenching or grinding one's teeth when not chewing.
-Calculus
Sometimes referred to as tartar, tartar is a hard deposit that forms on teeth. Calculus is the result of the calcification of debris around the teeth, and it can be avoided by practising meticulous oral hygiene. Once calculus has formed, it is difficult to eradicate, and requires the services of a dental therapist or hygienist in most cases.
-Absolute arch
A complete arch refers to the teeth of the upper or lower mandible in their entirety.
-Consultation
A dental consultation to evaluate potential treatment options. Appointments may include an examination, x-rays, and photographs, as well as a frank discussion and explanation, if necessary.
-Crown
Crowns can be manufactured from a variety of materials, including porcelain, porcelain fused to metal, and gold. The majority of crowns that are not visible in the mouth are white in pigmentation.
-CBCT scan
Cone Beam Computed Tomography is a sophisticated x-ray technique that generates three-dimensional images of the mandible. Due to their three-dimensional nature, these images can only be observed on a computer screen.
-Definitive refurbishments
The definitive restoration refers to the ultimate implant-supported crown, bridge, or denture fabricated during the treatment process. The restoration will require routine maintenance and may require replacement.
-The administration of dental anaesthetics
Anaesthesia (Greek: ) means without sensation, which includes pain. The majority of dental anaesthetics are administered via injection into the affected area. Rarely, procedures may be performed while you are unconscious; this is known as a general anaesthetic.
-Dental implant
An implant is an artificial "tooth root." The majority of implants are composed of metal, with titanium or titanium alloys being the most prevalent. Implants are surgically inserted into the jawbone in order to support crowns and bridges or to stabilise dentures.
-Dentures
Dentures are removable, custom-made replacement teeth. Typically, they are composed of acrylic or acrylic and cobalt chromium.
-Extraction
Extraction of teeth is the removal of teeth.
-Extraction position
The space left after tooth extraction.
Effective implantation
A functioning implant is one or more implants that are capable of supporting a dental restoration, such as a crown, bridge, or denture, and biting.
-Therapeutic tissue regeneration
A procedure that promotes the regeneration of soft tissue (gums) and may be used to improve the aesthetics around teeth or crowns.
-Gum disease
Soft tissue disease surrounding teeth. Gingivitis is the common name for gingival inflammation; it is a response to the deposition of plaque and, in most cases, can be treated with rigorous oral hygiene.
-Periodontal disease
Gingivitis can develop into periodontitis, a more severe form of gum disease, if left untreated. Periodontitis causes bone loss and can threaten the survival of a tooth or teeth.
-Immediate loading
Providing a temporary crown or bridge concurrently with implant implantation. Not all patients are appropriate candidates for this treatment.
-Inferior dental nerve
This nerve, sometimes known as the inferior alveolar nerve, travels through a bony canal in the lower jaw and provides sensation to the lower teeth, before emerging from bone as the mental nerve, which provides sensation to the lower lip.
-Combination toothbrushes
A small interdental brush with typically a single tuft of filaments. This can be used as an alternative to dental floss for cleansing between teeth and around implants.
-Maximum sinus
A hollow, air-filled space located just above the upper premolars. This varies in size from person to person and grows throughout one's lifetime.
-Molars
The upper and lower third molars on both sides of the mandible.
-Onlay anastomosis
When bone is taken from another area of the body, such as the hip (rarely), jaw, or behind the molars, and grafted to a deficient area.
-Osseointegration
Osseointegration is the bonding or fusion of an implant and bone, which typically takes several weeks to months.
-Plaque
Plaque is a soft, sticky, colourless film of bacteria that forms continuously on teeth and gums and can harden into calculus if not removed daily by practising good oral hygiene (brushing, flossing, etc.).
-Premolars
The two teeth located on both sides of the mandible in front of the molars.
-Reline procedure
During a relining procedure, a soft or firm material is used to correct the fitting surface of a denture following an extraction or surgery.
-Removable overdenture
A removable denture that is supported by implants but can be removed by the patient for cleansing.
-Restorations
The restoration may consist of a filling, a crown, a bridge, or a denture. It restores the tooth or teeth to full functionality.
-Rejuvenating phase or appointment
This phase follows the surgical phase of the treatment plan, typically a few weeks to a few months after a sufficient degree of recuperation. In the majority of instances, this will involve obtaining impressions so that the technician(s) can fabricate the definitive restoration.
-Sinus augmentation
A surgical procedure in which bone regenerative material is inserted into the sinus to stimulate the formation of new bone in order to enhance the available bone height for implant placement.
-Sterile conditions
In this context, sterility refers to the absence of bacterial contamination. We can never achieve absolute sterility, but we must always strive to achieve as near as possible to a sterile working environment. This includes the use of autoclaves to sterilise all nondisposable instruments as well as drapes and robes to isolate working surfaces and personnel.
-Titanium
This biocompatible metal is used to manufacture implants. Titanium has been utilised for decades in medical procedures, including hip replacements.
-Treatment scheme
A report outlining the patient's dental implant procedure, including the proposed treatment timeline and expenditures. The purpose of this guide is to provide an overview of standard dental implant treatment. Each individual's treatment plan for dental implants will be customised by Norfolk Dental Specialists in terms of cost, duration, and method of care delivery.
How Bite Splints and Dental Occlusion Adjustments Can Help with Relief from Ear Tinnitus and TMJ Pain?
Living with ear tinnitus and TMJ pain can be incredibly challenging, affecting both our physical and emotional well-being. However, as a dentist, I am here to shed light on a lesser-known solution that can provide relief for these conditions. By addressing occlusal interferences and utilising custom-made bite splints, we can effectively reduce ear ringing and alleviate TMJ pain, ultimately improving your quality of life.
Living with ear tinnitus and TMJ discomfort can be extremely difficult and detrimental to our physical and mental health. But as a dentist, I'm here to highlight a less well-known treatment that helps alleviate these symptoms. We can successfully minimise ear ringing and relieve TMJ pain by correcting occlusal interferences and using personalised bite splints, thereby enhancing your quality of life.
Recognising the Relationship:
It is impossible to emphasise the complex relationship between tooth occlusion and ear tinnitus or TMJ pain. Occlusal interferences, which lead to imbalances in the jaw joint, might be the result of misaligned teeth, a bad bite, or persistent grinding and clenching. These imbalances can result in ear tinnitus and TMJ pain, which can cause discomfort, decreased functionality, and a general decline in wellbeing.
Occlusal Adjustments for Relief:
Making occlusal modifications is one of the most important strategies for dealing with these problems. A qualified dentist can find interferences and imbalances by thoroughly analysing your teeth's alignment and evaluating your bite. We can eliminate tension on the jaw joint and the resulting symptoms of ear tinnitus and TMJ pain by making exact changes to your dental occlusion.
Customised Bite Splints:
When occlusal modifications alone may not be enough to relieve pain, using bite splints can be quite helpful. Bite splints, commonly referred to as removable appliances, are made-to-measure tools used to realign the jaw and offer a secure, comfortable position for biting. These splints not only relieve pressure on the jaw joint but also guard the teeth from wear and tear caused by clenching and grinding. Patients who use bite splints on a regular basis report less ringing in their ears and TMJ pain, as well as enhanced jaw mobility and better oral health.
Getting Professional Assistance:
Consult with a dental expert who specialises in occlusion and temporomandibular joint issues if you are experiencing ear tinnitus, TMJ pain, or TMJ clicking. Our knowledgeable staff at Clinic For Implant & Orthodontic Dentistry, located at 7 Chapel Road in Worthing, BN11 1EG, is committed to offering these patients individualised attention and successful treatments. To take the first step towards receiving the assistance you need, schedule a consultation right away.
Despite the difficulty of dealing with ear tinnitus and TMJ pain, relief is possible with the correct dental treatment. An expert dentist can significantly lessen ear ringing and TMJ symptoms by resolving occlusal interferences and deploying bespoke bite splints. Reach out to our dentist office right now to start your journey towards a better, pain-free life and don't let these conditions hold you back.
Diet Advise following Full Jaw Implant Surgery.
All-on-4 implant surgery is a treatment option for those with periodontal disease or tooth decay. The procedure involves placing implants in the jaw to support a full arch of replacement teeth. After the surgery, patients can expect some adverse effects, including minimal oozing, swelling, tense jaw and facial muscles, and site-specific pain. These symptoms are temporary and can be managed with over-the-counter pain medication. It is important to rest for the first three to four days, then gradually resume normal activities and exercise.
All-on-4 implant surgery is a thorough and successful treatment for periodontal disease and tooth decay, in cases where an entire upper or lower arches are missing or irreparable. Before the benefits of All-on-4 implant surgery take full impact, you can anticipate certain adverse effects after surgery. Possible symptoms include:
- Minimal oozing
- Swelling
- Tense jaw and facial muscles
- Sore throat and/or trouble swallowing
- Site-specific pain
If you experience adverse effects, they are transient and often subside after one week. Any pain or discomfort can be alleviated with over-the-counter drugs such as Paracetamol, Aspirin, or Ibuprofen.
It is very imortant to rest for the first three to four days. After that period of time, and as tolerated, you may resume normal activities and exercise.
However, dietary limitations last longer. These constraints can be divided into two time categories:
- First three weeks after surgery
- From three to six weeks after surgery
Knowing which foods are acceptable to eat following the surgery are crucial, as they will help you with the following;
- Reduces the impact of any pain and/or swelling
- Promotes a rapid recovery
- Maximise the benefits of your All-on-4 operation
If you already have dietary restrictions due to a medical condition (such as diabetes), you should visit a physician or trained nutritionist for advice.
Blender for soft food diet - after surgery, a blender will be your best buddy.
3 Weeks Post-Surgery: Eating on a Liquid Diet
Your mouth, jaw, and throat are likely to be painful for either a few days or up to three weeks after surgery, however any pain or swelling will progressively lessen. As a result, eating might be unpleasant or challenging. During this time a liquid diet without chewing is required.
Here are some considerations to make during this time period;
- The majority of pain post surgery is felt immediately after the surgery. It may be challenging to open your mouth and swallow. If your jaw feels rigid, making it difficult to open your mouth, try massaging it with an ice pack.
- Liquids can be consumed shortly after surgery. In the first 48 hours, you should only consume cool liquids. If you intend to consume something hot, do so until after the anaesthetic has worn off and all bleeding has ceased. It is best to avoid hot or spicy liquids until the third or fourth postoperative day.
- Hydration is key! It's important to consume a great deal of fluids, but in tiny quantities and often throughout the day. Once the anaesthetic has worn off and you feel comfortable enough, you should consume clear fluids shortly after surgery. Fluids will restore and maintain the tissue's moisture for optimal healing, regardless of whether there is drainage following the procedure.
- You will experience hunger as a result of consuming just liquids and avoiding solid foods for the first three weeks following All-on-4 implant surgery. In addition, optimal nutrition is necessary to avoid illness and accelerate recovery. Ensure that the fluids you consume during the day are nutrient-rich and that you consume them often. Given that you have just undergone oral surgery, it is expected that your intake would be lower than usual. However, you must bear in mind that nourishment is essential to healing, and without it you may experience a delay. Following is a list of foods that can be consumed during the first one to two weeks following surgery.
Important - do NOT use a straw when consuming liquids or liquidised food. The sucking movement might loosen blood clots, causing more bleeding and delaying the healing process.
What foods may I consume during this time?
There are numerous liquid foods that can be consumed during the first three weeks following All-on-4 implant surgery. The following are examples of consumable liquids;
- Soup broths (bouillon - beef, poultry, and vegetable)
- Creamy soups (without solids)
- Coconut liquid
- Kefir drinks
- Fruit juices
- Tea/coffee
- Warm cocoa
- Milk, including all forms of cow milk, from fat-free to whole
- Milk derived from nuts or peas
- Milkshakes
- Yogurt drinks
- Meal substitute shakes
- Protein shakes
- Smoothies
- Sodas
- Gelatine (e.g. Jelly)
- Custard
- Ice cream
- Frozen fluids, like fruit ices or popsicles
- Frozen yoghurt
When consuming milkshakes, yogurt drinks, fresh fruit jucies, smoothies and protein shakes, the consistency should be light enough for easy sipping. As the days pass and you feel you can stomach it, you can consume heavier shakes.
When you need to increase your calorie intake, put the following foods in your shakes:
Whites of powdered eggs, milk powder products, instant breakfast mixes (e.g., instant oatmeal), butter, margarine, or oil, sugar, syrup, or honey, or brewing yeast.
Sample Menu for first three Weeks After Surgery
Following is an example of a one-day menu for a fluid diet immediately following All-on-4 surgery. It is vital to note that you should have snacks to ensure that you receive the necessary nutrients and calories for recuperation.
Breakfast
- Fruit juice or smoothie
- Cup of tea or coffee
- Yogurt
- Glass of water
Breakfast Snack
- Glass of fruit juice
- Glass of water
Lunch
- Meal replacement drink
- Cup of broth
- Jelly
- Glass of water
Dinner
- Cup of broth or soup that has been strained
- Cup of fruit juice
- Yogurt
- Glass of water
Evening Snack
- Ice cream or frozen yogurt
- Warm cocoa
- Glass of water
3 weeks to up to 6 weeks after surgery; A soft food diet
After the pain subsides, you will feel more capable of transitioning from a liquid diet to a soft food diet. During the weeks and months following surgery, it is vital to remember that your jaw is still mending and the implants are attempting to integrate.
The process by which the jaw creates a biological bond with the implant screws is known as osseointegration. To ensure that this occurs correctly, you must continue to monitor your diet.
During the inital three months, you MUST avoid consuming meals that are - heard, chewy or crunchy and that require less chewing.
What foods may I consume during this time?
After three weeks, the following are examples of things you can add to your diet;
- Anything that is mashed or puréed, such as - mash potato, fruits, vegetables
- Everything soft, such as - bananas and melons
- Everything in a can and lacking skin and seeds
- Anything baked or cooked to a tender texture
- Soft breads, cakes
- Cooked pasta (soft)
- Noodles
- Quinoa, cous cous
- Eggs - poached, scrambled
- Pureed sauces
Example Menus for three weeks to six weeks:
This is a sample menu for a one-day soft food diet after surgery. It is vital to note that you should have snacks to ensure that you receive the necessary nutrients and calories for recuperation.
Breakfast
- Scrambled eggs on soft bread
- Fruit juice or smoothie
- Cup of tea or coffee
- Yogurt
- Glass of water
Breakfast Snack
- Bowl of soft fruit
- Glass of fruit juice
- Glass of water
Lunch
- Soup
- Stir fry with soft vegetables and noodles
- Jelly
- Soft fruits
- Glass of water
Dinner
- Meat cooked to a tender texture with mashed potato
- Cup of fruit juice
- Soft cake wirh custard or cream
- Glass of water
Several Important Suggestions for the Recuperation Period
Utilize a food blender or processor. If you can combine some of your favourite foods, you can better appreciate the fluid/soft food diet restrictions during the first several weeks of recuperation.
If you enjoy your food, you are more likely to consume sufficient calories and nutrients to help the healing process. Take initiative. When you decide to undergo this procedure, begin investigating what foods you can and cannot consume. This can include recipes for various shake and smoothie varieties. This can also help you stock up on food before surgery so that you are prepared to eat after you get home to recover.
Observe your body. Adjust your intake if you ever feel like you are not getting enough or are perhaps getting too much. Ask relatives for support. And get ~plenty of rest.
How about...
What about unmentioned details? You have learnt primarily what meals you can eat and a small amount about those you should avoid. But there are certain foods and beverages that we are commonly questioned about;
- Do not consume nuts or similar items - these will be far too hard and crunchy for your jaw
- Avoid hot and spicy liquids 24 to 48 hours after the surgery
- During the recovery phase, excessive alcohol consumption should be avoided, as alcohol consumption can impair the dental implants.
You can always consult the dental surgeon should you have any enquiries.
A budget alternative to fixed full jaw implant prosthesis is a snap on denture (overdenture) starting from £2500. By Dr Amir Mostofi DDS, Dip. , MSc.
Overdentures, also referred to as snap-on dentures, are a type of denture that attaches to a few dental implants placed in the jaw bone. Compared to conventional dentures, they have a number of advantages, such as better stability, retention, and a more realistic bite. Additionally, they offer increased durability, do not need adhesives, and aid in maintaining the jaw bone. The price range begins at £2500.
A budget alternative to fixed full jaw implant prosthesis is a Snap-on denture (overdenture) starting from £2500.By Dr Amir Mostofi DDS, Dip. ,MSc.
Here, I would like to explain about a cheaper alternative that our practice, Clinic for Implant and orthodontic dentistry is providing. A budget alternative to fixed full jaw implant prosthesis is a snap on denture (overdenture) whith the cost starting from £2500 in UK (at the time of writting). Some patients would like to have a full jaw implant restored fixed prosthetics. However, the cost of such treatment is beyond their reach. The cost of fixed dental implants for a full jaw restoration can vary depending on several factors, such as the number of implants needed and the experience level of the surgeon. However, on average, a fixed full jaw restoration with fixed dental implants can cost between £12000 to £25000 in UK. A practical alternative is option of overdenture (snap on denture). The cost of Snap-on dentures for a full jaw restoration is typically less expensive. The cost can vary depending on the number of dental implants needed and the materials used for the denture. However, on average, the cost for a full jaw restoration with a Snap-On denture can range from £2500 to £12000 in United Kingdom. This cost is more affordable for many patients.
Snap-on dentures, also known as overdentures, are a type of denture that snaps onto a small number of dental implants in the jaw bone. This type of denture offers a number of benefits over traditional dentures, which rest on the gums and are held in place by suction or adhesives.
One of the main benefits of snap-on dentures is improved stability and retention. Traditional dentures can slip and move around in the mouth, causing discomfort and making it difficult to speak and eat. Snap-on dentures, on the other hand, are securely attached to the dental implants, which anchor them firmly in place. This means that snap-on dentures do not slip or move around in the mouth, which greatly improves the ability to speak and eat.
Another benefit of snap-on dentures is that they provide a more natural-feeling bite. Traditional dentures can change the way the jaw and teeth align, which can cause discomfort and even jaw pain. Snap-on dentures, however, are anchored to the jaw bone, which helps to maintain the natural alignment of the jaw and teeth. This can help to reduce discomfort and jaw pain.
Another benefits of snap-on dentures is that they do not require adhesives to hold them in place. Traditional dentures rely on adhesives to keep them in place, which can be messy and unpleasant to use. Snap-on dentures, on the other hand, are anchored to the jaw bone and do not require adhesives to stay in place. This makes them more convenient and comfortable to wear.
In addition, snap-on dentures can help to preserve the jaw bone. Traditional dentures rest on the gums and rely on suction to stay in place. Over time, this can lead to bone loss in the jaw, which can cause the dentures to fit poorly and make the face appear sunken. Snap-on dentures, however, are anchored to the jaw bone and help to preserve bone and maintain a more youthful appearance. Snap-on dentures, also known as overdentures, are a more cost-effective option for full jaw restoration compared to fixed dental implants. While both options can provide a secure and stable solution for missing teeth, the cost of fixed dental implants can be significantly higher.
Another factor to consider is the maintenance costs. Fixed dental implants require regular check-ups and cleaning like natural teeth, but snap-on dentures are easy to clean and maintain, which can save patients on additional costs in the long run.
It's worth noting that the final cost of the treatment will depend on the individual case, and it's important to consult with a dental professional to get an accurate estimate of the cost. In conclusion, Snap-On dentures offer a number of benefits over traditional dentures, including improved stability and retention, a more natural-feeling bite, greater durability, no need for adhesives, preservation of jaw bone, more budget friendly and easy to clean. While they may require more upfront costs, snap-on dentures are a more secure, durable, and comfortable option for those in need of dentures.
"Dental Bite Splints: A Comprehensive Guide to Relief, Protection, and Improved Oral Health" - By Dr Amir Mostofi DDS, Dip. MSc
A dental bite splint is a small, detachable device worn over the teeth to assist reduce pain and suffering brought on by bruxism, TMJ disorders, and other abnormalities with the bite. These splints can be tailored to fit a person's mouth and are often constructed of acrylic or other hard plastic materials.
Bruxism is a condition in which a person unintentionally clenches or grinds their teeth, frequently when they are asleep. Numerous issues, such as tooth deterioration, jaw pain, migraines, and facial muscle pain, may result from this. In order to reduce pressure and strain on the jaw muscles and joints, which can cause pain and discomfort, bite splints work by giving the teeth a smooth, even surface to rest on.
What are dental bite splint?
A dental bite splint is a small, detachable device worn over the teeth to assist reduce pain and suffering brought on by bruxism, TMJ disorders, and other abnormalities with the bite. These splints can be tailored to fit a person's mouth and are often constructed of acrylic or other hard plastic materials.
Bruxism is a condition in which a person unintentionally clenches or grinds their teeth, frequently when they are asleep. Numerous issues, such as tooth deterioration, jaw pain, migraines, and facial muscle pain, may result from this. In order to reduce pressure and strain on the jaw muscles and joints, which can cause pain and discomfort, bite splints work by giving the teeth a smooth, even surface to rest on.
The jaw joint and the muscles that govern the jaw are both impacted by TMJ disorders. These conditions can make it difficult to bite and chew, as well as create pain and discomfort in the jaw, cheeks, neck, and shoulders. By helping to stabilise the jaw and redistribute the power of biting and chewing, bite splints can assist to reduce these symptoms.
Bite splints come in a variety of designs and forms, each with a distinct function. Hard splints, soft splints, occlusal guards, and orthopaedic splints are the most popular varieties. Hard splints are designed to offer a sturdy surface for the teeth to rest on and are composed of acrylic or other hard plastic materials. They are typically worn at night and can aid in reducing bruxism and TMJ disease symptoms. On the other side, soft splints are created to be more comfortable to wear and are constructed of softer materials like silicone or rubber. They are typically worn during the day and offer a temporary fix for people who have dental work or missing teeth, as well as relief from the signs and symptoms of bruxism and TMJ disorders. In order to protect the teeth from harm when participating in sports or other physical activities, occlusal guards are similar to hard splints. Orthopedic splints, on the other hand, can be worn for a longer amount of time and are intended to assist address misaligned bites or other abnormalities with the bite.
Each patient's bite splint is normally constructed specifically for them by a dental practitioner. To identify the root of the patient's bite issues, the procedure starts with a dental examination and bite analysis. The dentist will then make a model of the patient's mouth using impressions of the patient's teeth. The bite splint is then created using the model as a guide and materials and methods tailored to the patient's requirements.
The usage of a bite splint has several advantages, including the reduction of pain and suffering brought on by bruxism and TMJ conditions, defence against teeth grinding and clenching, stabilisation of the jaw and correction of misaligned bites, and enhancement of sleep. However, using a bite splint has some potential drawbacks as well, such as initial discomfort while getting used to wearing the splint, difficulty speaking or eating while wearing the splint, the need for routine cleaning and maintenance of the splint, and the potential for tooth movement or changes in the bite if the splint is not properly fitted or maintained.
A dental bite splint is an effective tool for people who suffer from pain and discomfort brought on by teeth grinding, TMJ disorders, and other bite-related problems. These splints can offer comfort, safeguard teeth, and enhance general dental health. If a biting splint is the best course of therapy for you, it's crucial to speak with a dentist who can also correctly fit and maintain the splint to maximise its effectiveness.
While bite splints can frequently help with the pain and discomfort brought on by bruxism and TMJ issues, it's crucial to treat the underlying issue if you want to experience long-lasting relief. This may entail dietary adjustments, stress reduction measures, or the application of additional therapies like mouthguards or dental appliances.
It's critical to maintain appropriate dental hygiene while wearing a biting splint in addition to treating the underlying causes of bite issues. To do this, you should frequently brush your teeth, floss them, and visit a dentist for cleanings and checkups. To ensure their efficiency and durability, bite splints should also be frequently cleaned and stored in a safe place when not in use.
If any discomfort or problems develop while using a bite splint, it is extremely crucial to speak with a dental expert. If the splint is not offering the required relief or if it is causing any discomfort or problems, it may need to be changed or replaced.
Although bite splints can be a beneficial therapy choice for many patients, they might not be appropriate for all patients. Before beginning use of a bite splint for treatment, it is crucial to discuss any worries or queries with a dental practitioner.
Bite splints can improve general oral health in addition to reducing pain and discomfort. Bite splints can assist to prevent tooth damage and maintain the health of the teeth and gums by shielding the teeth from clenching and grinding. Additionally, they can aid in jaw stabilisation and bite alignment correction, enhancing the mouth's overall functionality and attractiveness.
In general, bite splints can be a helpful therapy choice for those who are in pain or uncomfortable due to teeth grinding, TMJ disorders, or other bite-related problems. Although utilising a biting splint may have some downsides, for many people, the advantages of comfort and better oral health may outweigh these concerns. To ensure the success of the bite splint, it is crucial to work closely with a dental professional to choose the best course of treatment and to properly fit and maintain the appliance.
Wisdom teeth extractions- By Dr Amir Mostofi DDS, Dip. MSc
teeth:Wisdom teeth The four permanent adult teeth known as wisdom teeth are placed at the top and bottom back corners of your mouth. A wisdom tooth extraction is a surgical procedure to remove one or more of these teeth.
If an impacted wisdom tooth is causing you pain, an infection, or other dental problems, you will likely need to have it extracted. Wisdom teeth can be extracted by an oral surgeon or a dentist.
Even if impacted teeth are not currently causing problems, some dentists and oral surgeons may recommend extraction to prevent future complications. reactions, pre- and postoperative guidelines
Overview
The four permanent adult teeth known as wisdom teeth are placed at the top and bottom back corners of your mouth. A wisdom tooth extraction is a surgical procedure to remove one or more of these teeth.
You'll probably need to have a wisdom tooth removed if it is impacted, causing you pain, an infection, or other dental issues. An oral surgeon or a dentist can remove a wisdom tooth.
Even if impacted teeth aren't currently causing issues, some dentists and oral surgeons advise wisdom tooth extraction to avoid potential future issues.
How did it get done?
The final permanent teeth to erupt in the mouth are the wisdom teeth, sometimes known as third molars. Between the ages of 17 and 25, these teeth typically erupt. Some individuals never get wisdom teeth. Others do not experience any issues when their wisdom teeth erupt naturally, just like their other molars did.
Wisdom teeth that don't have enough room to erupt into the mouth or develop normally are known as “impacted” wisdom teeth. Impacted wisdom teeth may partially or completely fail to emerge.
A wisdom tooth that is impacted can:
Toward the following tooth, grow at an angle (second molar)
Grow at an angle with your mouth's roof.
Grow at a right angle to the neighbouring teeth, appearing to "lye down" in the jawbone.
Like other teeth, they can grow straight up or down, but they cannot come out of the jawbone.
Impacted wisdom teeth issues
If your impacted wisdom tooth causes issues like these, you'll probably need to have it extracted:
Pain
food and debris becoming stuck behind the wisdom tooth
Infections or gum disease (periodontal disease)
tooth decay in a wisdom tooth that has partially erupted damage to the tooth next to it or the surrounding bone
creation of a cyst (cyst) around the wisdom tooth that is filled with fluid
problems with the orthodontic procedures used to straighten other teeth
Avoiding future dental issues
Dental experts disagree on the benefits of removing impacted wisdom teeth when they are not causing issues (asymptomatic).
With impacted wisdom teeth, future issues are impossible to forecast. Here is the justification for pre-emptive extraction, though:
Even wisdom teeth without symptoms could be diseased.
It's frequently challenging to reach the tooth and give it the required cleaning if there isn't enough room for it to erupt.
In younger adults, severe wisdom tooth issues are less common.
Surgery-related problems and difficulty for older patients are also possible.
Risks
The majority of wisdom tooth extractions don't cause long-term issues. However, sometimes a surgical procedure that involves making an incision in the gum tissue and bone excision is necessary to remove an impacted wisdom tooth. Rare problems may arise from:
When the post-operative blood clot is lost from the site of the surgical wound, a painful dry socket or exposed bone results (socket)
bacterial or food-particle-trapped infection in the socket
damage to the bones, sinuses, nerves, or teeth close
How you get ready
The procedure might be carried out in the dental office. However, your dentist could advise seeing an oral surgeon if your tooth is severely impacted or if the extraction calls for a complex surgical procedure. Your surgeon may advise sedation in addition to local anesthesia to numb the area and make you more comfortable throughout the treatment.
Issues to raise
You might wish to ask your oral surgeon or dentist the following questions:
What number of wisdom teeth must be extracted?
What kind of anaesthetic am I going to get?
How difficult do you anticipate the process to be?
How long will the process probably take?
Have the other teeth been harmed by the impacted wisdom teeth?
Is there a chance I could sustain nerve damage?
What other dental procedures might I require in the future?
How long does it take to fully recover and resume daily activities?
Getting ready for surgery
Almost always, wisdom tooth extractions are done as outpatient procedures. You will therefore return home that day. The staff at the hospital or your dentist will give you information on what to do the day before and after your scheduled procedure. Query these things:
Is it necessary for me to plan for a ride home following the procedure?
Do I need to fast and refrain from eating, drinking, or both? If yes, when should I start?
Can I take my prescribed drugs before the procedure? If so, when can I start taking a dose before the procedure?
Is there anything I should stay away from taking before the operation?
What to anticipate?
Throughout the process
Depending on how comfortable you are and how complicated the removal of your wisdom teeth is predicted to be, your dentist or oral surgeon may choose one of three types of anesthesia.
Options consist of:
A local anesthetic
Each extraction location receives one or more injections of local anaesthetic from your dentist or oral surgeon. Your dentist or surgeon will probably numb your gums with a chemical before administering an injection. During the tooth extraction, you are awake. You won't feel any discomfort, although feeling some pressure and movement.
Anesthesia and sedation.
Through an intravenous (IV) line in your arm, your oral surgeon or dentist administers sedative anesthesia to you. During the surgery, a sedation anaesthetic subdues your consciousness. You won't remember much of the process and won't experience any pain. Additionally, you'll need local anesthesia to make your gums numb.
General sedation
You might be given general anaesthesia in certain circumstances. You might either have an IV line in your arm or inhale medication through your nose. You subsequently go unconscious. Your medicines, breathing, temperature, hydration intake, and blood pressure are all continuously monitored by your surgical team. You won't feel any pain and won't remember the process. Additionally, local anaesthetic is administered to ease discomfort following surgery.
Surgical procedure
When removing wisdom teeth, your dentist or oral surgeon will:
Creates a cut in the gingival tissue to reveal the tooth and bone
bone that prevents access to the dental root is removed
if it's easier to remove the tooth in sections, divide it.
takes out the tooth, removes any dental or bone debris from the area where the tooth was removed.
Closure of the wound with stitches is done to aid in healing, albeit it is not always necessary.
Apply gauze to the extraction site to stop bleeding and promote the formation of a blood clot
Following the procedure
After the procedure, you are transferred to a recovery room if you underwent general or sedation anaesthesia. If you had local anaesthetic, you would probably spend the short recovery period in the dental chair.
Follow the advice from your dentist as you recover from your procedure.
Bleeding.
Blood may ooze on the first day following wisdom teeth removal. Spitting excessively should be avoided to prevent removing the blood clot from the socket. As instructed by your dentist or oral surgeon, replace the gauze over the extraction site.
Management of pain.
An over-the-counter pain treatment like Paracetamol or Ibuprofen or a prescription painkiller from your dentist or oral surgeon may help you manage pain. If bone was removed during the treatment, prescription pain medication might be especially beneficial. A cold compress applied to your jaw may help provide pain relief.
Bruising and swelling.
As advised by your dentist or surgeon, use an ice pack. Your cheek swelling often goes down in two to three days. It can take a few more days for bruises to heal.
Activity.
Plan to rest for the rest of the day after your procedure. The following day, return to your regular routine, but refrain from any strenuous exercise for at least a week to prevent losing the blood clot from the socket.
Beverages.
Water is important to drink after surgery. In the first 24 hours, refrain from consuming any alcoholic, caffeinated, carbonated, or hot beverages. For at least a week, refrain from drinking using a straw since the sucking motion could push the blood clot out of the socket.
Food.
For the first 24 hours, stick to soft foods such as yogurt or applesauce. Once you can tolerate soft meals, start eating them. Avoid things that can stick in the socket or irritate the wound by avoiding hard, chewy, hot, or spicy foods.
Smoking
Smoking should be avoided for at least 72 hours following surgery, and ideally for longer. Don't chew tobacco for at least a week if you do. After oral surgery, using tobacco products might hinder recovery and raise the possibility of problems.
Stitches.
You might not have any stitches at all or have stitches that fall out in a few weeks. Make an appointment to have your stitches removed if they need to be taken out.
When to call a surgeon or dentist?
If you suffer any of the following warning signs or symptoms, which could point to an infection, nerve damage, or other severe problem, call your dentist or oral surgeon right away:
Breathing or swallowing challenges
A lot of blood
Fever
Severe pain that is not alleviated by painkillers as prescribed
Swelling that gets worse two or three days later
A foul taste in your tongue that saltwater rinsing cannot cure
Pus in the socket or leaking from it
Enduring numbness or a loss of sensation
Nasal discharge with blood or pus
If problems arise, speak with your dentist or oral surgeon..
What is an overdenture?- By Dr Amir Mostofi DDS, Dip. MSc
An overdenture is a cheaper removable substitute for a full jaw fixed implant treatment. A denture with one or more teeth, prepared roots, or implants covered at the base is known as an overdenture. Any removable dental prosthesis known as an overdenture is one that covers and rests on one or more natural teeth that are still present, their roots, and/or dental implants. Overdentures can be implant- or conventionally tooth-supported. Alveolar bone is found to be preserved and the process of total edentulism is postponed. For senior individuals who have lost some teeth but not all, making them qualified for a set of full dentures, an overdenture is typically employed. The overdenture is detachable and not fixed in the mouth. Overdentures have the advantage over complete dentures in that the roots that are still in the maxilla (upper jaw) or mandible (lower jaw) protect the top or lower jaw's bone, reducing bone resorption.
Implants may support an upper or lower overdenture.
The most frequent number of implants used to stabilise an upper denture is 4, despite the fact that there is little evidence to conclusively demonstrate the appropriate number of implants for stabilising an upper overdenture.
Support for a mandibular overdenture was improved when two implants were present rather than just one implant.
The patients could also chew much better and was overall more pleased with the overdenture.
Sometimes a metal bar connecting implants will enhance retention of an overdenture.
The patient's overall satisfaction with the overdenture increased along with how much better they could chew. Initially chewing abilities are decreased, however when the overdenture has been fitted for a year, the chewing cycle improves.